Dr Thomas Crowhurst
Pulmonary function testing

Pulmonary function testing is an essential component of the assessment of most respiratory disorders and can be required on a repeated basis as part of monitoring for response to treatment or disease progression.
There are many different tests that can be undertaken to assess lung health, with some of the most common explained below.
- Spirometry:
- Gas transfer:
Gas transfer (also called ‘diffusing capacity’) seeks to assess how efficiently the lungs can transfer inhaled gas into the bloodstream and is thus a surrogate for their capacity to absorb oxygen. This is a very important test to assess for damage of the lung tissue itself, as can occur in emphysema and interstitial lung disease among many other disorders.
- Body plethysmography:
Body plethysmography involves the patient sitting in a special glass chamber and breathing through a spirometer, enabling measurement of lung volumes. This allows determination of total lung capacity (the volume of gas within the lungs) as well as subdivisions of lung volumes, which can be particularly relevant in obstructive lung disease where gas trapping within the lungs can be problematic.
- Maximal inspiratory and expiratory pressures:
- Arterial blood gas analysis:
- Six minute walk test:
- Altitude simulation test:
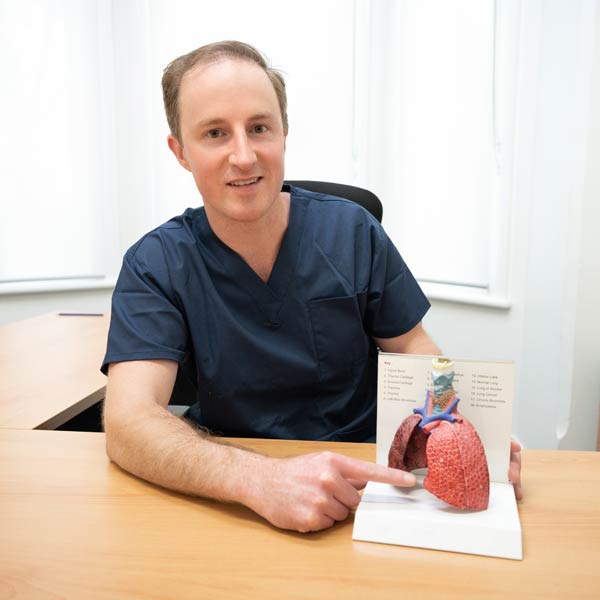
Dr Crowhurst will explain why certain pulmonary function tests will be helpful in your particular situation. He will show you the results of your pulmonary function tests, explain these to you and outline the significance of the findings in your individual circumstances. He will note whether any repeat testing may be helpful. Copies of the results will be provided to you and, with your consent, to any other doctors involved in your care.
Dr Crowhurst reports pulmonary function testing at Respiratory SA in Kent Town, Northern Respiratory in Elizabeth, and at the Lyell McEwin Hospital and Modbury Hospital.